There is a high potential for nosocomial spread of SARS-CoV-2. Reports from Italy showed that 20% of healthcare workers became infected with COVID-19 and many died. This CNN article reports that almost 10% of all Italian COVID patients are health care workers. It is inevitable that not only will the number of US patients infected with coronavirus increase, but that the number of US healthcare workers with COVID will substantially increase as well. We know that infections in general will provide immunity to repeat infections, but that reinfections with COVID (or COVID “relapses”) have been documented and, according to one study from Hong Kong, coronavirus may remain present in our systems for 5 weeks or more.
We don’t know which of us may have been infected already because testing in most parts of the country is limited or nonexistent and because more than 80% of COVID cases show mild or no symptoms.
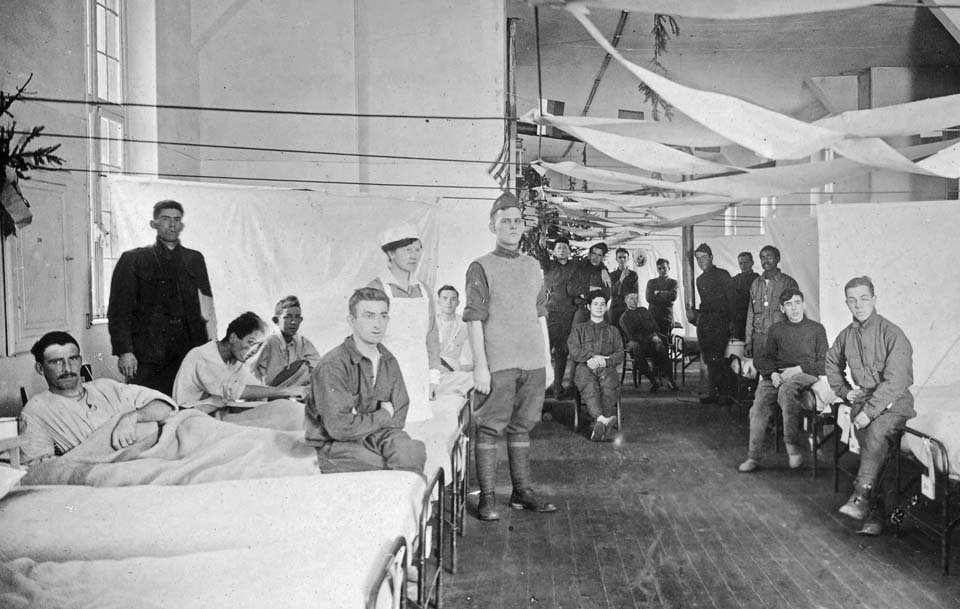
What we desperately need to know is what to do after someone has been infected and presumably recovers from COVID-19. This is especially true for healthcare providers. As we prepare for the tsunami of patients, we also need to prepare our “MASH units.”
Post Recovery Issues to Address
Should a COVID-infected healthcare provider continue to see patients? If so, under what conditions? Absence of fever? Full mask/gown/gloves? Mask only? Must the patient be informed that the provider is COVID positive? Will patients accept care from a COVID positive provider? We generally don’t inform patients about a provider’s infection with influenza, HIV, or other diseases. Should COVID be different?
If a COVID-infected healthcare provider is not permitted to see patients, under what conditions may the healthcare provider return to clinical duties? Is the provider out until viral testing shows undetectable levels? Will we be able to do multiple tests to confirm undetectable levels?
Should we follow a “symptoms-based” approach? In other words, should any patient known to be infected with COVID remain out of work until “symptoms resolve”? Many patients have few if any symptoms from COVID infections and we know that the virus may remain in the system much longer than symptom resolution.
In the case of medical providers, what if providers contract COVID, but only develop minor symptoms? Should all providers be tested and then should those with positive tests be excluded from patient care? If so, how often should the tests be taken? We know that the turnaround time for testing currently is many days at worst to approximately 8 hours at best. What should the providers do while waiting for test results? How do we make sure that the providers haven’t been infected between the time that they are tested and the time that the results are reported?
If we use a “symptoms-based” approach, do we follow the minimum 7 days currently recommended by the CDC? Do we use 14 days? If not, what should be the timeframe? Should isolation times begin when a patient began having symptoms or when COVID is diagnosed? In other words, if a patient has had a cough and fever for one week, but tests positive, it is possible that the disease will have resolved. Should that patient still wait 14 days before returning to work? The admittedly small hydroxychloroquine/azithromycin study from France showed that only 12% of untreated COVID patients had undetectable viral load at 6 days.
After a COVID patient has convalesced, then what? When can the patient go back to work? Should there be any work restrictions?
When should healthcare providers be able to resume clinical duties? Most hospitals require proof of titers for MMR/Hep B/etc. and allow providers who have received influenza shots to treat patients without using protective gear. Providers who have not had seasonal flu shots are usually required to wear masks. We don’t yet have an assay for SARS-Cov-2 titers. How should we determine when a provider who did have COVID is no longer infectious? What if a provider has a documented COVID infection then subsequent testing shows absence of viral RNA? At that point, should infection resolution and immunity be assumed?
We can’t even provide testing to many ICU patients right now due to lack of available tests. Will we be able to perform repetitive testing on any patients? If so, who will pay for the costs? With any testing, we must also consider the sensitivity of such testing. There will always be false positives and false negatives with any test and it would be naïve to assume that all patients with a negative test results do not have COVID.
As with those receiving influenza or who have recovered from influenza, do we assume that the providers who have recovered from COVID are now “immunized” and safe to see possible/suspected COVID patients without extensive protective gear? Or do we use full protective gear until what little reserves of gear that remain have been exhausted? From Hong Kong studies, it appears that a small subset of patients may become reinfected with COVID.
We need to carefully consider the policies we develop for patients suffering from and recovering from COVID infections. Strict return to work policies will encourage all workers to under-report their symptoms and to avoid testing so that they can continue working – which will only hasten the spread of disease. Strict “return to work” policies will also quickly deplete our entire system of necessary employees and will overwhelm noninfected healthcare professionals during unprecedented patient surges.
We must decide how to reincorporate COVID patients back into the workforce. If we ostracize those with the disease, the ranks of all workers will quickly dwindle and we will rapidly lose this fight.